 |
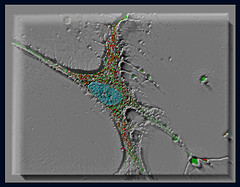
| Human fibroblast (Photo credit: glyn_nelson) |
Dermal fillers are an important tool in the armamentarium of an aesthetic dermatologist in the management of ageing skin these days and its popularity is on the rise. But among dermal fillers the safe materials are short lasting while long lasting materials are not really safe. Certain materials that claim to be safe and long lasting by fibroblast activation do not have appropriate physico-mechanical properties. They are ‘bony hard’ and rarely even deposits bone! An ideal filler material should be biodegradable, non-cytotoxic, enhance fibroblast adherence and proliferation. It should also have ideal physico-mechanical properties. Scientists from University of Akron, Ohio doing research on biopolymers have stumbled upon such a material.[1] It is still early days and the research team has not even declared it as a probable dermal filler material.
‘Pseudo’ poly (aminoacids) such as L-Tyrosine polyurethanes (LTUs) have been synthesized by the structural modification of poly (aminoacids) by incorporation of non-peptide bonds into the polymer’s backbone. These bioplolymers have superior mechanical properties (particularly their excellent elasticity) without cytotoxic degradation products. They augment fibroblastic adhesion and proliferation that is even tunable to certain extend by subtle changes in the polymer structure.
I dare go to the extent of predicting it as a next generation hair loss treatment because of its ideal rheological properties as a scaffold for blood-vessel generation as I hypothesised before.
GlaxoSmithKline has a unique topical steroid molecule called GW870086 in the pipeline that could change the way we treat inflammatory skin disorders.[2] A modification of the 17α position of the steroid nucleus resulted in a molecule that retained the effect on anti-inflammatory targets while having minimal impact on the expression of other known target genes responsible for the side effects. The properties of GW870086 were compared to fluticasone propionate (FP) using a range of model systems, including extensive gene expression profiling. Murine models of irritant-induced contact dermatitis showed promising results. If the same efficacy and safety profiles can be demonstrated on humans as well, it may fulfill our long quest for a safe topical steroid.
Special thanks to Dr Yun of University of Akron and Dr Uings of GSK and their respective teams for the details.

- Machine learning-based BOTOX API - April 11, 2023
- Skinmesh: Machine learning for facial analysis - November 10, 2020
- Free Dermatology EMR for Machine Learning and Artificial Intelligence - January 2, 2020




Leave a Reply